Developed by Reframing Autism’s Intersectional Advisory Committee with
Dr Alexandra Johnston*, June 2024, and edited by Dr Melanie Heyworth
Reviewed by Raelene Dundon, Liz Baird, and Phyllis Bogopa
This Position Statement on diagnosis is divided into parts. The first is a summary of Reframing Autism’s position on Autism diagnosis and the second is the research and experiential background which informs this statement.
See the appendix for three lived experience testimonials to support the statement. There are also two plain language articles to complement the official position statement on self-identification and diagnostic privilege.
Reframing Autism acknowledges the complexity of the diagnostic process and the multiple individuals who have deep investment in the formal assessment and diagnosis of Autism. This Position Statement encompasses both formal, clinical diagnosis of Autism, as well as self-identification without formal confirmation, and the principles encoded here apply to diagnosis across the lifespan. We appreciate this statement is lengthy, so throughout, to aid navigation, texts in bold indicate our key positions. Texts in italics represent lived experience testimonies offered in support of this Position Statement.
Reframing Autism endorses a formal assessment and diagnostic process that is accessible, safe and trauma-informed, timely, government subsidised, accurate, and helpful to individuals and their families and carers. We specifically endorse this process when it is approached from the individualised, strengths-based, citizenship, and human rights frameworks that are fundamental to the biopsychosocial model of disability, and when diagnostic assessment is used to support an Autistic individual to be their best Autistic self.
We call for rigorous and standardised neuro-affirming training (including continuing professional development) in autism and autism assessments for clinicians who conduct diagnostic assessments. This would ensure that trained, knowledgeable and experienced clinicians can conduct diagnostic assessments that account for intersectional identities, a diversity of presentation, co-occurring conditions, and cultural realities, and eschew deficits-based, stereotypical and outdated understandings of Autistic presentations. Thus, we advocate for culturally responsive and neurodiversity-affirming diagnostic processes, in which clinicians work in partnership with the individual, and their families and carers, to provide accessible, appropriate, helpful, and respectful information and supports tailored to individual and family needs and strengths.
Reframing Autism questions the efficacy and accuracy of diagnostic tools which were developed without Autistic guidance or input, and which rely on deficits-based, pathologised and outdated understandings of Autism. We thus call for research into standardised diagnostic tools, which are genuinely co-produced with the Autistic community, so that diagnostic tools and the diagnostic process are strength-based and neuro-affirming, and are attuned to the many variations of Autistic processing, communicating and functioning. We also advocate for updating the language in diagnostic manuals to be strengths-based and affirming. We reject the ‘top-down’ provision of an assessment and diagnostic process that (intentionally or unintentionally) ‘others’ Autistic people, aims to suppress intrinsic or authentic Autistic behaviours, or implies that a non-autistic neurology is superior or preferable to an Autistic one.
We stress the critical importance of quality, co-produced, and neuro-affirming post-diagnostic support for Autistics of all ages, including that provided by the Autistic community. However, we spotlight the high need for support and resources specifically tailored to the growing population of Autistic adults identified later in life – sometimes referred to as the “lost generation” – who face considerable inequality in support (Howlin, 2021).
Reframing Autism endorses self-identification as a valid decision for Autistic individuals. We acknowledge self-identification is a self-determined process, enacted by and through an Autistic individual’s autonomy, competence and volition. Reframing Autism rejects the stigmatisation, marginalisation, invalidation, and othering faced by Autistic individuals who have chosen to self-identify.
We often use the term “diagnosis” as is if it was a word that we understand completely and therefore needs no examination. Yet, diagnoses serve social functions and are shaped by social forces (Jutel, 2009). Diagnoses aren’t static categories: they respond to changing social norms and expectations and respond to developing medical knowledge; they are fluid and adapt to meet the fluidity of ever-changing social standards and improved medical expertise. Diagnoses, then, have ideological effects, and there is a complex interplay between social structures, political ideologies, and the designation of what is “acceptable” and “normal”, and what is not; what is “deviant” or “disordered”, and what is not. The mechanism of diagnosis is a “cultural expression” of the boundaries that society deems normal, and what it deems as problematic or needing treatment (Jutel, 2009). To illustrate this point, we can trace the history of homosexuality in the Diagnostic and Statistical Manual of Mental Disorders (DSM) from its inclusion as a sociopathic personality disturbance in the original edition of the DSM from 1952, to its removal altogether from the DSM-III in 1974, reflecting society’s evolving recognition that homosexuality had no place being ‘diagnosed’ as a ‘mental disorder’. In other words, diagnoses actively evolve over time to reflect evolving cultural values. Diagnoses, then, exert an important material force, by allowing disease and disorder to be framed by, and in turn frame, social and cultural values (Jutel, 2009). So, diagnoses – and diagnostic manuals like the DSM – reflect sociocultural norms and expectations, and they are limited and shaped by the power dynamics which prioritise some forms of “knowing” (e.g., research, professional) over others (e.g., experiential).
The current clinical approach to Autism is pathologised, medicalised and deficits-based. In the DSM-5-TR “Autism Spectrum Disorder” is characterised as a set of deficits and impairments and behaviours that deviate from the norm and are pathologised as “disordered” because they are “atypical” or “abnormal”. But as a diagnosis, Autism too, is evolving. In the earliest DSMs, Autism was not its own diagnosis, but a subset of childhood schizophrenia. It wasn’t separated from schizophrenia until 1980 in the DSM-III where it was listed as Infantile Autism, and then Autistic Disorder. Asperger’s wasn’t introduced as a subset of Autistic Disorder until 1994 in the DSM-IV, and it was then removed in 2013 in the DSM 5. In DSM 5, the specific Autism-related “deficits” are grouped into a dyad of impairments, around social communication and interactions on the one hand, and restricted and repetitive behaviours, activities and interests on the other. Thus, although we are a long way from depathologising Autism, it is certainly not a stagnant or static diagnosis.
You can read more about Autism as a changing diagnosis in Tim Chan’s reflection on his lived experience of diagnosis over time (see the Appendix, Testimonial 1).
The diagnostic assessment of Autism is thus a complex undertaking, involving systemic processes by which a practitioner or diagnostic team may confer a clinical diagnosis of Autism Spectrum Disorder (ASD), according to specific diagnostic criteria (e.g., DSM-5-TR, 2022 or ICD-11, 2019). As our knowledge of Autism deepens, and as society evolves to embrace and accept neurodivergences, these diagnostic descriptions and criteria will continue to evolve in response. Importantly, the diagnostic criteria, and the associated measures used to assess whether an individual meets those criteria, are not informed by, or co-produced with, the Autistic community, and they are rarely sensitive to complex and diverse Autistic presentations, which may be shaped by culture, experiences, co-occurring conditions, intersectionality, gender and race.
You can read more about the current best practice for Autism diagnosis in the “National Guideline for the assessment and diagnosis of autism in Australia”.
Reframing Autism advocates for diagnostic criteria and measures to be co-produced with the Autistic community to more adequately and accurately represent our experiences. Our community deserves diagnostic clinicians and teams who are sufficiently able to respond to and engage with each individual’s complex history and identity in strengths-based, neuro-affirmative ways.
Adults who think they might be Autistic often face big hurdles in getting a formal diagnosis. Self-identification is where an individual identifies themselves as Autistic, without seeking a formal diagnosis from healthcare professionals (Fellowes, 2024). The process of self-identification is often protracted and involves deep consideration, thought and contemplation to explore if an individual aligns themselves, or feels resonance, with not only the Autistic characteristics as set out in the diagnostic manuals, but equally, the lived experiences of other Autistic people. Learning more about how an individual’s Autistic characteristics “fit” with their true self can enable individuals to develop deeper self-awareness, which can lead to a clearer conceptualisation of and alignment with an Autistic identity (Alper et al., 2023; Swan, 2017).
There are many reasons for why an individual may choose or prefer to self-identify, rather than pursue a formal diagnosis, although this can be due to being unable to access appropriate or accessible diagnostic services, with financial, cultural and geographical barriers often cited. Equally, lack of practitioner knowledge and skills (both at a general health and specialist level) may impede formal diagnosis, which is especially for true for multiply marginalised individuals (Alper et al., 2023; Fletcher-Watson, 2024; Helms, 2022; Lewis, 2017; Sarett, 2016). Other individuals choose not to pursue formal diagnosis because of previous medical traumas, time constraints, or the emotional toll.
Importantly, some Autistic people are simply ambivalent about the formal diagnostic process; they self-identify because they do not feel they need the “approval” of a medical clinician to adopt an Autistic identity. For some, formal diagnosis represents a systemic power imbalance, since medical professionals are perceived as holding the power in determining who is Autistic and who is not, rather than an individual themselves contributing to a shared discourse about their experience as an Autistic person (Fletcher-Watson, 2024). In this regard, diagnostic processes centralise power within the medical establishment, with medical professionals perceived as gatekeepers to diagnostic services, contributing to feelings of exclusion and marginalisation (Alper et al., 2023).
Reframing Autism supports the range of individual choices in formal diagnosis and self-identification, recognising that either path can contribute to the enhancement of autonomy, empowerment and wellbeing of Autistic individuals. We endorse the shift in the existing “balance of power” in diagnosis and service provisions towards a needs-based model of individual support and care.
We nevertheless acknowledge that there are specific benefits and barriers associated with both formal diagnosis and self-identification, which are explored further below.
Diagnosis, in the formal sense, is costly and time-consuming, with benefits as well as possible negative impacts, and there are significant barriers to accessing formal diagnosis.
Nevertheless, a positive experience of the diagnostic assessment process can help form a sense of positive identity, for an individual and their family, and reframe feeling “broken” or “wrong” (Gaffney, 2020; Harmens et al., 2022). Done well, the diagnostic process is shown to support individuals and their families to develop understanding and acceptance, and to provide confirmation and validation for experiences of difference which in turn can improve wellbeing (Fletcher-Watson, 2024; Huang et al., 2023). Additionally, the formal diagnostic process can be an access point for appropriate medical care for co-occurring conditions, and is a potential starting point for accessing support and services (Gaffney, 2020), like the National Disability Insurance Scheme (NDIS) in Australia, which can then facilitate funding to promote individuals and families to thrive.
Diagnosis also affords Autistic individuals’ legally mandated access to educational and workplace accommodations, which can often open opportunities for inclusion and equitable participation. Examples of workplace adjustments include modifying the physical environment and offering flexible work hours to support social, processing and sensory needs; examples of educational accommodations include the adaption of curriculum, and access to universal design for learning (Davies et al., 2022; Fletcher-Watson, 2024).
Although Autistic people report experiences of stigma, discrimination and exclusion because of their Autistic identity (Botha et al., 2022), a diagnosis can equally promote an understanding of Autistic individuals (Fletcher-Watson, 2024). Moreover, diagnosis can support a feeling of community and belongingness, through connection with other Autistic people and the broader Autistic community (Crompton et al., 2020; Fletcher-Watson, 2024; Lilley et al., 2023), since a diagnosis often promotes increased social interaction with other Autistic people or time spent in Autistic spaces. Experiencing such belongingness has positive correlation with individual wellbeing (Crompton et al., 2020; Crane et al., 2021).
Despite the potential benefits, evidence from both research and lived expertise indicates that there are significant barriers for individuals and families to access diagnostic assessment.
For a lived experience testimony recounting a formal diagnosis journey, see the Appendix, Testimonial 2 by Jenny Mitchell.
Cost and time
A key barrier to accessing a formal diagnosis with a medical professional is cost (Estrin et al., 2021; Fisher et al., 2023), which is compounded by lengthy wait times to access the range of health care providers an individual may need to access for obtaining a referral for diagnosis (Alpers et al., 2023; Fletcher-Watson, 2024).
Reframing Autism advocates for timely, government-subsidised (e.g., Medicare-covered) diagnostic assessment so that cost and time are not barriers.
Gender
Unfortunately, some medical professionals still erroneously believe that ‘only males’ can be Autistic, and gender can therefore be a barrier to diagnosis (Estrin et al., 2021; Rabbitte et al., 2017). Compared with males, Autistic females often encounter more difficulties during the diagnostic process (Duvekot et al., 2017; Dworzynski et al., 2012), typically receiving diagnosis at a later age (Kirkovski et al., 2013; Rutherford et al., 2016), and experiencing a higher risk of misdiagnosis, diagnostic overshadowing, or delayed diagnosis, which can result in significant negative consequences for the individual’s wellbeing (Hull & Mandy, 2020). This illustrates the potentially pervasive and detrimental impact of clinicians’ stereotyped perceptions of Autistic characteristics (Gesi et al., 2021; Harmens et al., 2022), as well as outdated diagnostic markers grounded in traditional understandings of Autistic behaviours (Kirkovski et al., 2013; Kopp & Gillberg, 2011). Additionally, diagnostic procedures are often not sensitive to Autistic masking or camouflaging, which is reported to be higher in Autistic women (Hull et al., 2020), and medical professionals may overlook an Autism diagnosis due to their inexperience and lack of expertise knowledge (Takara et al., 2015).
Over time, the rates of Autism diagnosis have increased, reflecting a broadening of diagnostic criteria to include individuals with diverse presentations (Brugha et al., 2011; Saemundsen et al., 2013). Indeed, more adult women are seeking and receiving Autism diagnoses compared to men, suggesting that women are more likely to be missed at a younger age (Happé & Frith, 2020; Happé et al., 2016).
Parents of girls and young women observe many barriers to diagnosis, including lack of information, limited resources, and clinician bias, and girls may be less likely to be referred for assessment or experience longer waiting times (Estrin et al., 2021).
Reframing Autism advocates for the co-design of Autism diagnostic tools that are nuanced, responsive to intersectionality, and reflect the lived experiences of the full breadth of the Autistic community, including women, girls, and gender divergent people, since gender remains a significant barrier at all levels of identification and diagnosis for non-males (Hull & Mandy, 2020; Milner et al., 2019).
Intersectional inequities and Autistic Indigenous Australians
Access to diagnosis is unequal, with observable disparities based on race, ethnicity, culture, gender, wealth, and socioeconomic status. Comparisons across nations reveal wide variations in diagnostic rates, highlighting global inequities, and the sociocultural biases of health providers can act as a barrier to formal diagnosis, which include biases around gender, race, colour and culture (Alper et al., 2023).
In particular, intersectional barriers faced by racial and ethnic minority individuals, and families of Autistic children are rooted in ideological, economic, and political domains (Mallipeddi & VanDaalen, 2022; Singh & Bunyak, 2022). These barriers vary based on race, language, and culture. For example, Autistic children in Black, Indigenous, and people of colour (BIPOC) communities are diagnosed later and misdiagnosed more frequently than their white peers (Aylward et al., 2021; Fisher et al., 2023; Perryman et al., 2018). This delay and misdiagnosis are linked to systemic biases and a historical context of oppressive treatment for Black and Brown disabled individuals (Morgan et al., 2022), and an increasing body of research literature evidences the experiences of racism and marginalisation within diagnostic processes (e.g., Alyward et al., 2021; Fisher et al., 2023; Jegatheesan et al., 2010; Pearson & Meadan, 2018; Sakai et al., 2019; Zuckerman et al., 2014)
Significant marginalisation is experienced by Autistic Aboriginal and Torres Strait Islander (First Nations) individuals compared to their non-Indigenous counterparts (Bailey & Arciuli, 2020). This marginalisation is exacerbated by socio-economic disparities that contribute to unequal health and education outcomes, leading to poorer long-term outcomes for First Nations people. A high likelihood of First Nations individuals being undiagnosed or misdiagnosed can be attributed to several barriers to accessing support, including long waitlist times, high service costs, unnecessarily complicated access pathways, limited awareness of support services, and geographical isolation (McDonald & Zetlin, 2004). Additionally, some First Nations individuals, and their families and carers, report experiencing racism and disrespect from some service providers through rushed consultations, inappropriate use of jargon, and a lack of respect, making them feel dismissed and their views irrelevant. This disrespect is further compounded by predominantly non-Indigenous service providers giving advice that is not culturally responsive or appropriate in the family’s context. Carers feel subjected to inflexible government rules, such as rigid eligibility criteria, which prevent them from accessing appropriate supports. Out-of-pocket expenses, including food and transport costs, further burden carers, many of whom have had to exit the labour force or reduce work hours to provide care, impacting their physical and psychological health (Green et al., 2016).
Reframing Autism calls for a culturally responsive, knowledgeable, collaborative, and respectful intersectional diagnostic approach to address racial, cultural, and structural obstacles effectively.
Age (late diagnosis)
Delayed diagnoses are more prevalent in middle aged and older people (Hickey et al., 2018; Huang et al., 2023). Adults seeking a formal Autism diagnosis face multiple barriers, including anxiety, cost, limited access to adult specialists, and a general lack of awareness of diverse presentations of Autism among healthcare professionals (Crane et al., 2018; Lewis, 2020; Taylor et al., 2017). Differences in capabilities to describe characteristics, fear of not being believed or understood, lack of rapport or mistrust of healthcare professionals, stigma, and the complexity of the healthcare system further exacerbate these barriers (Lewis, 2017).
Other barriers inherent in adult diagnosis are executive functioning challenges and social and sensory anxiety (e.g., making appointments, attending in-person assessments); interoceptive and alexithymic differences (e.g., difficulty in verbalising traits, feelings and experiences; Trammell et al., 2013); a dearth of clinicians specialising in adult Autism evaluation (Zerbo et al., 2015); fear of not being believed or being dismissed by clinicians (Crane et al., 2018; Lewis, 2017); misdiagnosis, the prevalence of co-occurring conditions, and diagnostic overshadowing (Au-Yeung et al., 2019, Happé et al., 2016; Lai et al., 2015; Trammell et al., 2013); reliance on childhood experiences to establish the historical presence of traits (Lai et al., 2015; Trammell et al., 2013), and multiple marginalisation (e.g., LGBTQIA+ identity, physical disabilities, Indigeneity; Alper et al., 2023; Fisher et al., 2023; Mallipeddi & VanDaalen, 2022).
“I cannot overstate how much my blindness has and continues to impact my Autism and ADHD.” (Stormy Meiying Liu).
Reframing Autism advocates for Autism assessment to be conducted by skilled clinicians who are experienced in, and knowledgeable of, the complexities inherent to adult presentations, especially for marginalised and intersectional groups.
The barriers to formal diagnosis highlighted above necessitate a re-examining of diagnostic measures and clinical biases to ensure for inclusivity and accessibility (Kirkovski et al., 2013), and to address existing inequalities. We call for co-designed measures that draw on a breadth of experiential expertise and are sensitive and responsive to the many intersectional complexities experienced by Autistic people.
Reframing Autism strongly recommends incorporating coproduced and co-developed formal education about Autism into standard training curricula and continuing professional development for all health and mental health professionals, and ensuring that continuing education opportunities about Autistic people are available for health and mental health practitioners and psychotherapists to reduce the systematic and systemic “blind spot” in recognising and providing respectful, meaningful support to Autistic individuals, and their families and carers.
Reframing Autism urgently advocates for addressing these systemic limitations, as an imperative which may likely improve healthcare access for Autistic individuals, and life outcomes more broadly.
Reframing Autism, then, calls for a formal diagnostic process that is timely and financially accessible, undertaken by respectful, skilled and knowledgeable clinicians who possess nuanced and community-informed understandings of Autistic lived experiences, and using co-designed diagnostic measures that are culturally responsive and pay due attention to the range of intersectionalities in the Autistic community, in accessible and safe environments and contexts.
Reframing Autism maintains that done well, diagnosis can offer access to positive selfhood, agency, and self-acceptance, and can promote authentic Autistic lives. By bringing focus to Autistic needs, diagnosis can be an avenue for advocacy and support.
Self-identification circumvents many of the barriers of formal diagnosis, whilst still offering many of the benefits of formal diagnosis. Individuals who self-identify as Autistic report a feeling of liberation, stemming from an expanded self-awareness and associated increase in self-understanding (Fletcher-Watson, 2024; Park-Cardoso & Soares da Silva (2023). Indeed, self-identification as Autistic is often described as “I’ve come home” (Stormy Meiying Liu, 2024). Self-identification can help Autistic individuals make sense of their past and their personality, offering answers to life-long questions such as, “why am I like I am?” and “why am I different?” (Lewis, 2017; Park-Cardoso & Soares da Silva (2023). The process of self-identification is often lengthy and arduous, and involves the reflections of family members, friends, and acquaintances in addition to personal self-realisations (Overton et al., 2023), and extensive information gathering and research (Alper et al., 2023; Bury et al., 2022). Parents may come to identify as Autistic following their child’s diagnosis (Fletcher-Randle, 2022; Pohl et al., 2020; Thom-Jones, 2022), which often leads to shared identity formation in families, and a sense of belonging.
Ultimately, adults describe self-identification as promoting self-understanding, strengths identification, and the experience of belonging, whilst promoting wellbeing by reframing deficit-based messages and increasing self-compassion (Harmens et al., 2022). It may also offer an individual a sense of validation, welcome and belonging with the Autistic community, through connecting with people who are like ‘me’ (Lilley et al., 2023; Sarrett, 2016). Thus, some eschew the need for a formal diagnosis (Lewis, 2016).
“I knew deep down I was on the spectrum . . . I had found it (self-identification) a major relief, I’d found I could relate to the tests on-line and could see it clearly in myself. I had become the ‘undiscovered country’.” (Stormy Meiying Liu, 2024).
Reframing Autism, along with many in the Autistic and autism communities, holds that self-identification is equally as valid as a formal diagnosis. Autistic people have the self-awareness and self-knowledge to understand their neurotype, in the same way that non-autistic people recognise their neurotypicality. Most self-identified Autistic adults, after researching Autism, feel confident in their self-assessment (Sarrett, 2016).
“As I researched the work of actually Autistic people, watched their videos, read their blogs, and went out into Autistic spaces to meet more people like me, my understanding (and acceptance) of myself continued to crystalise. It was fellow Autistic people who opened the door to me developing self-knowledge. It was the Autistic community that led me through the dark to me developing self-knowledge. Psychiatry did not do that for me. And it would have been impossible for me to explore an Autistic identity if the community had been hostile toward the questioning or undiagnosed… So no, I don’t believe self-diagnosis is valid. I believe it is essential, just, and revolutionary.” (Price, 2023).
Reframing Autism recognises that self-identification later in life can be a significant turning point for Autistic adults, where self-emancipation through increased self-knowledge and awareness is often further developed through interactions with the collective self-knowledge of the online Autistic community (Park-Cardoso & Soares da Silva, 2023).
Nevertheless, we acknowledge that universal acceptance of self-identification by the full Autistic and autism communities is yet to transpire. Indeed Fellowes et al. (2023) highlight that the validity of Autistic self-identification is fiercely debated within the Autistic community and is considered by some to be divisive (Sarrett, 2016). For example, there is debate as to the extent to which an individual can accurately determine whether they meet diagnostic criteria (Sarrett, 2016), since self-identification often involves relying on individual, “subjective” judgment (Fellowes et al., 2023), rather than “objective” medical judgment.
Reframing Autism contends that, since diagnostic measures and clinician knowledge are not representative of diverse Autistic experiences and presentations, and are themselves ideologically framed, all processes of identification – formal or self – are subjective and interpretive.
Importantly, self-identification is often the only option available to individuals, including those who seek formal diagnosis. For example, older, employed women face significant challenges in being referred and assessed for a formal diagnosis (Overton et al., 2023), even though these individuals face similar social and economic challenges as their peers with a formal diagnosis. We emphasise the critical importance of providing support for individuals to access self-identification based on need and desire, a provision which could feasibly disrupt the dependency on formal diagnosis for service access and address disparities faced by disadvantaged groups (Fletcher-Watson et al., 2024).
Reframing Autism thus acknowledges the ongoing debate around self-identification. However, we fundamentally reject debate that compromises the human rights, citizenship, and wellbeing of Autistic individuals, and their families and carers. We maintain that self-identification is a vital mechanism for self-understanding, especially when formal diagnosis remains a privilege due to systemic barriers to access, and since diagnostic criteria and measures are, for some groups, inadequate. Moreover, we emphasise that self-identification is a viable and valid alternative to clinical diagnosis.
Because universal acceptance of self-identification is lacking, self-identified individuals can experience stigma and, in turn, a marginalised sense of identity (Alper et al., 2023; MacDonald, 2020). Self-identified individuals can find they are not always accepted as “Autistic” even within Autistic community. Equally unfortunately, the absence of a formal diagnosis can hinder the provision of financial and disability support (e.g., NDIS).
For more information on self-identification, see our information article here. For further explanation of why formal diagnosis is a privilege, see our information article here.
“The hardest part of this process was the lack of post-diagnostic support. All my efforts had gone towards a diagnosis, but now what? Finding effective supports… proved extremely difficult.” (Jenny Mitchell, Appendix Testimonial 2)
Reframing Autism notes that dissatisfaction with post-diagnostic support is prevalent among Autistic adults, with 79% expressing dissatisfaction with its availability and quality (Jones et al., 2014). This dissatisfaction is echoed by parents of Autistic children. Inadequate post-diagnostic support leads to less positive and less satisfactory diagnostic journeys, leaving individuals and families feeling directionless and lacking emotional support (Crane et al., 2018).
Reframing Autism acknowledges that improving the diagnostic process requires integrating the expertise of individuals, families, and professionals (de Clercq & Peeters, 2007) and providing respectful, meaningful, accessible and relevant supports during and after diagnosis or identification (Hennel et al., 2016). These supports should be tailored not only to the Autistic individual, but equally to their families, friends, colleagues, and peers, to ensure that the diagnostic process builds acceptance, autonomy, and authenticity.
“The most upsetting experience post-diagnosis has been the negativity and lack of support from some of those closest to me. Feeling I’m a burden because my capacity doesn’t match expectation, being offered prayer to heal my autism as though it’s a disease, having my decisions gas lit because I admit to struggling with executive functioning, and when my son received his diagnosis, receiving pity and assumptions that he would never be successful. Increasing society’s understanding and acceptance of neurodiversity and changing the conversation around autism would perhaps make it easier for me to disclose and fully embrace my autism diagnosis.” (Jenny Mitchell, Appendix Testimonial 2).
Reframing Autism also advocates for long-term, sustained post-diagnostic support, to acknowledge the time and complexity of an Autism diagnostic journey for both individuals and families. Post-diagnostic support should not be confined to a single moment, or time-period, after diagnosis or identification, but should rather be responsive to the needs, desires and aspirations of the individual, and their family and carers, and to what is needed to support people and families to thrive.
To read a lived-experience testimony reflecting on the impact of such lack of sustained support, see the account by Shazzy Tharby in the Appendix Testimonial 3.
* This Position Statement was developed by Reframing Autism’s Intersectional Advisory Committee (IAC), led by Dr Alexandra Johnston (Reframing Autism and Autism Centre of Excellence, Griffith University). We warmly acknowledge and thank the IAC and Dr Johnston, who have so generously shared their expertise and lived experience to inform this Position Statement. We equally thank Monique Lepouris (Master of Research Candidate, Macquarie University), who provided research assistance to support the Statement’s development.
Reframing Autism’s Intersectional Advisory Committee consists of a diverse group of people who represent some of the most marginalised communities within the Autistic population. Its members have lived experiences of complex communication needs, LGBTQIA+, CALD contexts, adoption, financial disadvantage, co-occurring psychosocial and physical disabilities, among others. IAC members have worked in ways that are accessible to them to produce resources for Reframing Autism, including the much-acclaimed Welcome Pack, and the position statement on diagnosis. We are indebted to their invaluable contribution to Reframing Autism’s work.
Alper, M. Rauchberg, J. S., Simpson, E., Guberman, J., & Feinberg, S. (2023). TikTok as algorithmically mediated biographical illumination: Autism, self-discovers, and platformed diagnosis on #autisktok. New Media & Society. https://doi.org/10.1177/14614448231193091
Au-Yeung, S. K., Bradley, L., Robertson, A. E., Shaw, R., Baron-Cohen, S., & Cassidy, S. (2019). Experience of mental health diagnosis and perceived misdiagnosis in Autistic, possibly Autistic and non-autistic adults. Autism, 23(6), 1508-1518. https://doi.org/10.1177/1362361318818167
Aylward, B. S., Gal-Szabo, D. E., & Taraman, S. (2021). Racial, ethnic, and sociodemographic disparities in diagnosis of children with autism spectrum disorder. Journal of Developmental & Behavioural Pediatrics, 42(8), 682-689. https://doi.org/10.1097%2FDBP.0000000000000996
Bailey, B., & Arciuli, J. (2020). Indigenous Australians with autism: A scoping review. Autism, 24(5), 1031-1046. https://doi.org/10.1177/1362361319894829
Botha, M., Dibb, B., & Frost, D. M. (2022). “Autism is me”: An investigation of how Autistic individuals make sense of autism and stigma. Disability & Society, 37(3), 427–453. https://doi.org/10.1080/09687599.2020.1822782
Brugha, T. S., McManus, S., Bankart, J., Scott, F., Purdon, S., Smith, K., Bebbington, P., Jenkins, R., & Meltzer, H. (2011). Epidemiology of autism spectrum disorders in adults in the community in England. Archives of General Psychiatry, 68(5):459–465. https://doi.org/10.1001/archgenpsychiatry.2011.38
Bury, S. M., Haschek, A., Wenzel, M., Spoor, J. R., & Hedley, D. (2022). Brief report: Learning about autism: Is the source of autism knowledge associated with differences in autism knowledge, autism identity, and experiences of stigma. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-022-05823-5
Crane, L., Hearst, C., Ashworrth, M., Davies, J., & Hill, E. L. (2021). Supporting newly identified or diagnosed Autistic adults: An initial evaluation of an Autistic-led programme. Journal of Autism and Developmental Disorders, 51, 892-905. https://doi.org/10.1007/s10803-020-04486-4
Crane, L., Batty, R., Adeyinka, H., Goddard, L., Henry, L. A., & Hill, E. L. (2018). Autism diagnosis in the United Kingdom: Perspectives of Autistic adults, parents and professions. Journal of Autism and Developmental Disorders, 48(11), 3761-3772. https://doi.org/10.1007/s10803-018-3639-1
Crompton, C. J., Hallett, S., Ropar, D., Flynn, E., & Fletcher-Watson, S. (2020). ‘I never realised everybody felt as happy as I do when I am around autistic people’: A thematic analysis of Autistic adults’ relationships with Autistic and neurotypical friends and family. Autism, 24(6), 1438-1448. https://doi.org/10.1177%2F1362361320908976
Davies, J., & Bagnall, C. (2024). “A good transition is just key”: The views and experiences of disability support staff in supporting Autistic students transition to university. Autism in Adulthood. https://doi.org/10.1089/aut.2024.0076
Duvekot, J., van der Ende, J., Verhulst, F. C., Slappendel, G., van Daalen, E., Maras, A., & Greaves-Lord, K. (2017). Factors influencing the probability of a diagnosis of autism spectrum disorder in girls versus boys. Autism, 21(6), 646-658. https://doi.org/10.1177/1362361316672178
de Clercq H., & Peeters, T. (2007). A partnership between parents and professionals. In J. M. Pérez, M. González, M. L. Comí, & C. Nieto (Eds.), New developments in autism: The future is today (pp. 310-340). Jessica Kingsley Publishing.
Dworzynski, K., Ronald, A., Bolton, P., & Happé, F. (2012). How different are girls and boys above and below the diagnostic threshold for autism spectrum disorders? Journal of the American Academy of Child & Adolescent Psychiatry, 51(8), 788-797. https://doi.org/10.1016/j.jaac.2012.05.018
Estrin, G. L., Milner, V., Spain, D., Happé, F., & Colvert, E. (2021). Barriers to autism spectrum disorder diagnosis for young women and girls: A systematic review. Review of Autism & Developmental Disorder, 8(4), 454-470. https://doi.org/10.1007/s40489-020-00225-8
Fellowes, S. (2024). Establishing the accuracy of self-diagnosis in psychiatry. Philosophical Psychology, 1–28. https://doi.org/10.1080/09515089.2024.2327823
Fisher, A. P., Lynch, J. D., Jacquez, F. M., Mitchell, M. J., Kamimura-Nishimura, K. I., & Wade, S. L. (2023). A systematic review examining caregivers’ of colour experiences with the diagnostic process of autism spectrum disorder. Autism, 27(4), 876-889. https://doi.org/10.1177/13623613221128171
Fletcher-Randle, J. E. (2022). Where are all the Autistic parents? A thematic analysis of Autistic parenting discourse within the narrative of parenting and autism in online media. Studies in Social Justice, 16(2), 389-406. https://doi.org/10.26522/ssj.v16i2.2701
Gaffney, J. C. (2020). ‘It’s autism, it’s just a name’: Exploring the impact of autism spectrum diagnosis with adolescent females using interpretative phenomenological analysis. Doctoral dissertation, University of Sheffield.
Gesi, C., Migliarese, G., Torriero, S., Capellazzi, M., Omboni, A. C., Cerveri, G., & Mencacci, C. (2021). Gender differences in misdiagnosis and delayed diagnosis among adults with autism spectrum disorder with no language or intellectual disability. Brain Sciences, 11(7), 912. https://doi.org/10.3390/brainsci11070912
Green, J. L., Rinehart, N., Anderson, V., Efron, D., Nicholson, J. M., Jongeling, B., Hazell. P., & Sciberras, E. (2016). Association between autism symptoms and family functioning in children with attention-deficit/hyperactivity disorder: A community-based study. European Child & Adolescent Psychiatry, 25, 1307-1318. https://doi.org/10.1007/s00787-016-0861-2
Happé, F. G., Mansour, H., Barrett, P., Brown, T., Abbott, P., & Charlton, R. A. (2016). Demographic and cognitive profile of individuals seeking a diagnosis of autism spectrum disorder in adulthood. Journal of Autism and Developmental Disorders, 46, 3469-3480. https://doi.org/10.1007/s10803-016-2886-2
Happé, F., & Frith, U. (2020). Annual Research Review: Looking back to look forward – changes in the concept of autism and implications for future research. Journal of Child Psychology and Psychiatry, 61(3), 218–232. https://doi.org/10.1111/jcpp.13176
Harmens, M., Sedgewick, F., & Hobson, H. (2022). Autistic women’s diagnostic experiences: Interactions with identity and impacts on well-being. Women’s Health, 18. https://doi.org/10.1177%2F17455057221137477
Helms, N. R. (2022). Seeing brains: Shakespeare, autism, and self-identification. In Redefining Disability, pp. 152-159. Brill. https://doi.org/10.1163/9789004512702
Hennel, S., Coates, C., Symeonides, C., Gulenc, A., Smith, L., Price, A. M. H., & Hiscock, H. (2016). Diagnosing autism: Contemporaneous surveys of parents needs and paediatric practice. Journal of Paediatrics and Child Health, 52(5), 506-511. https://doi.org/10.1111/jpc.13157
Howlin, P. (2021). Adults with autism. Changes in understanding since DSM-III. Journal of Autism and Developmental Disorders, 51(3). https://link.springer.com/article/10.1007/s10803-020-04847-z
Huang, Y., Trollor, J. N., Foley, K. R., & Arnold, S. R. (2023). “I’ve spent my whole life striving to be normal”: Internalized stigma and perceived impact of diagnosis in autistic adults. Autism in Adulthood, 5(4), 423-436. https://doi.org/10.1089/aut.2022.0066
Hull, L., Lai, M.-C., Baron-Cohen, S., Allison, C., Smith, P., Petrides, K., & Mandy, W. (2020). Gender differences in self-reported camouflaging in autistic and non-autistic adults. Autism, 24(2), 352-363. https://doi.org/10.1177/1362361319864804
Hull, L., & Mandy, W. (2017). Protective effect or missed diagnosis? Females with autism spectrum disorder. Future Neurology, 12(3), 159–169. https://doi.org/10.2217/fnl-2017-0006
Jegatheesan, B., Fowler, S., & Miller, P. J. (2010). From symptom recognition to services: How South Asian Muslim immigrant families navigate autism. Disability & Society, 25(7), 797–811. https://doi.org/10.1080/09687599.2010.520894
Jones, L., Goddard, L., Hill, E. L., Henry, L. A., & Crane, L. (2014). Experiences of receiving a diagnosis of autism spectrum disorder: A survey of adults in the United Kingdom. Journal of Autism and Developmental Disorders, 44, 3033–3044. https://doi.org/10.1007/s10803-014-2161-3
Jutel, A. (2009). Sociology of diagnosis A preliminary review. Sociology of Health & Illness, 31(2), 278-299. https://doi.org/10.1111/j.1467-9566.2008.01152.x
Kirkovski, M., Enticott, P. G., & Fitzgerald, P. B. (2013). A review of the role of female gender in autism spectrum disorders. Journal of Autism And Developmental Disorders, 43, 2584-2603. https://doi.org/10.1007/s10803-013-1811-1
Kopp, S., & Gillberg, C. (2011). The Autism Spectrum Screening Questionnaire (ASSQ)-Revised Extended Version (ASSQ-REV): An instrument for better capturing the autism phenotype in girls? A preliminary study involving 191 clinical cases and community controls. Research in Developmental Disabilities, 32(6), 2875-2888. https://doi.org/10.1016/j.ridd.2011.05.017
Lai, M. C., Lombardo, M. V., Auyeung, B., Chakrabarti, B., & Baron-Cohen, S. (2015). Sex/gender differences and autism: Setting the scene for future research. Journal of the American Academy of Child & Adolescent Psychiatry, 54(1), 11-24. https://doi.org/10.1016%2Fj.jaac.2014.10.003
Lewis, L. F. (2016). Exploring the experience of self-diagnosis of autism spectrum disorder in adults. Archives of Psychiatric Nursing, 30(5), 575-580. https://doi.org/10.1016/j.apnu.2016.03.009
Lewis, L. F. (2017). A mixed methods study of barriers to formal diagnosis of autism spectrum disorder in adults. Journal of Autism and Developmental Disorders, 47, 2410-2424. https://doi.org/10.1007/s10803-017-3168-3
Lewis, L. F. (2020). Barriers to formal diagnosis of autism spectrum disorder in adults. In F. R. Volkmar (Ed.), Encylopedia of Autism Spectrum Disorders (pp. 1-6). Springer Nature. https://doi.org/10.1007/978-1-4419-1698-3
Lilley, R., Lawson, W., Hall, G., Mahoney, J., Clapham, H., Heyworth, M., Arnold, S., Trollor, J., Yudell, M., & Pellicano, E. (2022). “Peas in a pod”: Oral history reflections on Autistic identity in family and community by late-diagnosed adults. Journal of Autism and Developmental Disorders. https://doi: 10.1007/s10803-022-05667-z
Mallipeddi, N. V., & VanDaalen, R. A. (2022). Intersectionality within critical autism studies: A narrative review. Autism in Adulthood 4(4), 281–289. https://doi.org/10.1089/aut.2021.0014
Maynard, D. W., & Turowetz, J. (2019). Doing abstraction: Autism, diagnosis, and social theory. Sociological Theory, 37(1), 89-116. https://doi.org/10.1177/0735275119830450
McDonald, T. A. M. (2020). Autism identity and the “lost generation”: Structural validation of the autism spectrum identity scale and comparison of diagnosed and self-diagnosed adults on the autism spectrum. Autism in Adulthood, 2(1), 13-23. https://doi.org/10.1089%2Faut.2019.0069
McDonald, C., & Zetlin, D. (2004). ‘The more things change…’: Barriers to community services utilisation in Queensland. Australian Social Work, 57(2), 115-126. https://doi.org/10.1111/j.1447-0748.2004.00126.x
Milner, V., McIntosh, H., Colvert, E., & Happé, F. (2019). A qualitative exploration of the female experience of autism spectrum disorder (ASD). Journal of Autism and Developmental Disorders, 49(6), 2389-2402. https://doi.org/10.1007/s10803-019-03906-4
Morgan, E. H., Rodgers, R., & Tschida, J. (2022). Addressing the intersectionality of race and disability to improve autism care. Pediatrics, 149 (Supplement 4). https://doi.org/10.1542/peds.2020-049437m
Overton, G. L., Marsa-Sambola, F., Martin, R., & Cavenagh, P. (2023). Understanding the self-identification of autism in adults: A scoping review. Review Journal of Autism and Developmental Disorders, 1-21. https://doi.org/10.1007/s40489-023-00361-x
Park-Cardoso, J., & Silva, A. P. S. da. (2023). Insistence on sameness for food space appropriation: An exploratory study on Brazilians with autism (self-)diagnosis in adulthood. Autism, 27(4), 938-951. https://doi.org/10.1177/13623613221121417
Pearson, J. N., & Meadan, H. (2018). African American parents’ perceptions of diagnosis and services for children with autism. Education and Training in Autism and Developmental Disabilities, 53(1), 17-32. https://www.jstor.org/stable/26420424
Perryman, T., Watson, L. R., & Chumney, F. (2018). Predictors of the age of autism spectrum disorder diagnosis: A North Carolina cohort. Autism & Developmental Language Impairments, 3. https://doi.org/10.1177/2396941517751892
Pohl, A. L., Crockford, S. K., Blakemore, M., Allison, C., & Baron-Cohen, S. (2020). A comparative study of autistic and non-autistic women’s experience of motherhood. Molecular Autism, 11(3). https://doi.org/10.1186/s13229-019-0304-2
Price, D. (2023, November 16). Self-diagnosis isn’t “Valid.” It’s liberatory. Devon Price. https://drdevonprice.substack.com/p/self-diagnosis-isnt-valid-its-liberatory
Rabbitte, K., Prendeville, P., & Kinsella, W. (2017). Parents’ experiences of the diagnostic process for girls with autism spectrum disorder in Ireland: An interpretative phenomenological analysis. Educational and Child Psychology, 34(2), 54-66. http://dx.doi.org/10.53841/bpsecp.2017.34.2.54
Ratto, A. B., Bascom, J., daVanport, S., Strang, J. F., Anthony, L. G., Verbalis, A., et al. & Kenworthy, L. (2023). Centering the inner experience of autism: Development of the self-assessment of autistic traits. Autism in Adulthood, 5(1), 93-105. https://doi.org/10.1089/aut.2021.0099
Rutherford, M., McKenzie, K., Johnson, T., Catchpole, C., O’Hare, A., McClure, I., Forsyth, K., McCartney, D., & Murray, A. (2016). Gender ratio in a clinical population sample, age of diagnosis and duration of assessment in children and adults with autism spectrum disorder. Autism, 20(5), 628-34. https://doi.org/10.1177/1362361315617879
Saemundsen, E., Magnússon, P., Georgsdóttir, I., Egilsson, E., & Rafnsson, V. (2013). Prevalence of autism spectrum disorders in an Icelandic birth cohort. BMJ Open, 20;3(6), e002748. https://doi.org/10.1136/bmjopen-2013-002748
Sakai, C., Mulé, C., LeClair, A., Chang, F., Sliwinski, S. K., Yau, Y., & Freund, K. M. Parent and provider perspectives on the diagnosis and management of autism in a Chinese immigrant population. Journal of Developmental & Behavioral Pediatrics, 40(4):257-265. https://doi.org/10.1097/DBP.0000000000000660
Sarrett, J. C. (2016). Biocertification and neurodiversity: The role and implications of self-diagnosis in Autistic xommunities. Neuroethics, 9, 23–36. https://doi.org/10.1007/s12152-016-9247-x
Silberman, S. (2015). Neurotribes. Allen & Unwin.
Singh, J. S., & Bunyak, G. (2019). Autism disparities: A systematic review and meta-ethnography of qualitative research. Qualitative Health Research, 29(6), 796-808. https://doi.org/10.1177/1049732318808245
Swan, M. (2017, July 17). 5 reasons I am self-identified as autistic. Hello Michelle Swan. https://hellomichelleswan.com/5-reasons-i-am-self-identified-as-autistic/
Takara, K., Kondo, T., & Kuba, T. (2015). How and why is autism spectrum disorder misdiagnosed in adult patients? – From diagnostic problem to management for adjustment. Mental Health in Family Medicine, 11, 73-88. DOI: 10.25149/1756-8358.1102011
Taylor L. J., Eapen, V., Maybery, M., Midford, S., Paynter, J., Quarmby, L., Smith, T., Williams, K., & Whitehouse, A. J. (2017). Brief report: An exploratory study of the diagnostic reliability for autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(5):1551-1558. https://doi.org/10.1007/s10803-017-3054-z
Thom-Jones, S. (2022). Growing in to Autism. Melbourne University Press.
Trammell, B., Wilczynski, S. M., Dale, B., & Mcintosh, D. E. (2013). Assessment and differential diagnosis of comorbid conditions in adolescents and adults with autism spectrum disorders. Psychology in the Schools, 50(9), 936–946. https://doi.org/10.1002/pits.21720
Zuckerman, K. E., Sinche, B., Mejia, A., Cobian, M., Becker, T., & Nicolaidis, C. (2014). Latino parents’ perspectives on barriers to autism diagnosis. Academic Pediatrics, 14(3), 301-308. https://doi.org/10.1016/j.acap.2013.12.004
Zerbo, O., Massolo, M. L., Qian, Y., & Croen, L. A. (2015). A study of physician knowledge and experience with autism in adults in a large integrated healthcare system. Journal of Autism and Developmental Disorders, 45(12), 4002-4014. https://doi.org/10.1007/s10803-015-2579-2
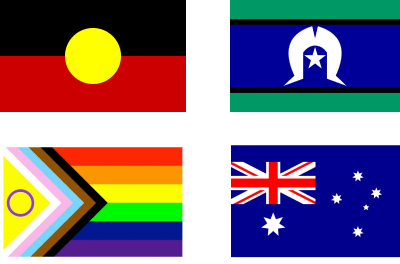
The Reframing Autism team would like to acknowledge the Traditional Owners of the lands on which we have the privilege to learn, work, and grow. Whilst we gather on many different parts of this Country, the RA team walk on the land of the Awabakal, Birpai, Whadjak, and Wiradjuri peoples.
We are committed to honouring the rich culture of the Aboriginal and Torres Strait Islander peoples of this Country, and the diversity and learning opportunities with which they provide us. We extend our gratitude and respect to all Aboriginal and Torres Strait Islander peoples, and to all Elders past and present, for their wisdom, their resilience, and for helping this Country to heal.